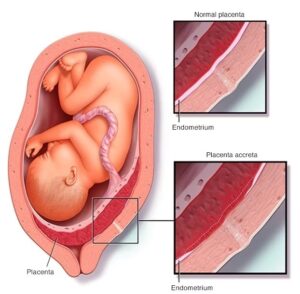
Placenta Accreta Spectrum (PAS) disorder results from abnormal placental implantation. It occurs when the placenta grows too deeply into the uterine wall during pregnancy and is most likely due to the increasing rates of late pregnancies and cesarean delivery.
Scarring in the uterus from a prior C-section or other uterine surgery is responsible for developing such condition and is regarded as high risk for ongoing or subsequent pregnancies. The incidences of PAS disorder is rising worldwide and cases have translated into figures of maternal morbidity & mortality.
PAS disorder, leads to postpartum hemorrhage and often the need for Hysterectomy. Maternal and neonatal outcomes generally tend to improve with timely diagnosis as the patient is managed by experts in the field of Obstetrics.
MRI is increasingly used for the evaluation of PAS disorder
-
- Diagnosis of PAS disorder should be sought during Anomaly scan (TIFFA/Level 2) at GA 18-22 weeks, yet PAS disorder is often not timely identified during pregnancy.
- Ultrasound is the 1st radiological modality which assesses the presence of PAS disorder. However MRI of Pelvis is often required for evaluation of areas difficult to visualize on ultrasound, and for correct assessment of the extent of Placenta Accreta.
- Ultrasound followed by an MRI Pelvis (for a thorough placental evaluation) is the gateway through which patients with PAS disorder are typically directed for proper patient management.
- In cases where ultrasound has already made a definitive diagnosis, MRI Pelvis is often used to plan for cesarean section delivery and peripartum hysterectomy.
Risk Factors
-
- Maternal age (placenta accreta is more common in pregnancies of women ≥ 35 years).
- Placenta position or prior history of cesarean delivery in the setting of placental previa (when the placenta partially or totally covers cervix) increases the risk of PAS disorder.
- Previous uterine surgery (such as myomectomy or any kind of uterine instrumentation).
- Multiple pregnancies greatly increase the risk of placenta accreta disorder.
- Use of cryo preserved embryo transfer for IVF pregnancies.
MRI Pelvis scan can demonstrate findings of PAS disorder as listed below;
-
- In 1st trimester, patients showing low implantation of gestational sac in the region of C-section scar, warrants for a dedicated assessment for PAS disorder.
- In 1st trimester, patients having teardrop configuration with a relatively empty appearing fundal endometrial cavity.
- In 2nd & 3rd trimester, the most common gray scale ultrasound signs of PAS disorder include loss of retro placental clear space.
Timing
Recommended time for PAS disorder assessment for Placenta Accreta by MRI is 24–30 weeks of gestation. The normal placenta exhibits homogeneous intermediate signal and is usually clearly distinct from the myometrium, which is more heterogeneous and hyper intense.
Before 24 weeks of GA, the placenta is immature and MRI performs poorly in diagnosing abnormal placentation. After 30 weeks of GA, the internal placental signal becomes more heterogeneous as the placenta matures. Thus, to minimize error, this study is best timed at 24–30 weeks GA.
Procedure & Safety Protocol
MRI of Pelvis is usually done with no evidence of adverse effects to the fetus.
However there are few safety concerns which should be adhered like;
-
- Rare heating effects due to RF pulse
- Acoustic injury to the fetus when exposed to the magnetic field.
Therefore scan should be performed strictly as per the set safety guidelines. Although no fetal harm has been reported with 1.5 T or less, there is a little risk involved at higher field strengths (3T).
Conclusion
Placenta Accreta Spectrum (PAS) disorder are becoming more frequent, largely because of the increasing rate of late pregnancy and cesarean delivery. Ultrasound is the first-line imaging modality for placental evaluation, but MRI Pelvis now plays an important role in antenatal diagnosis of invasive placentation and makes the treatment planning more effective to minimize maternal morbidity & mortality.
By carefully following the protocols of image acquisition, Ultrasound & MRI findings should be correlated as this reliably improves quality of diagnosis.

No comment